Finding the right Bipolar Disorder Medication can feel overwhelming, especially when symptoms swing between highs and lows that disrupt daily life. But treatment isn’t one-size-fits-all. The good news? Today’s options are broader and more personalized than ever.
In this guide, we break down the most common medications for bipolar disorder, how they work, and what to expect. Whether you or a loved one is navigating a new diagnosis or reassessing an old prescription, this overview will help you feel more informed and in control.
What Are the Main Types of Medications for Bipolar Disorder?
Bipolar disorder medication is designed to stabilize mood, reduce the intensity and frequency of episodes, and prevent relapse. Most treatment plans fall into one or more of the following categories:
Mood Stabilizers
These medications are often the foundation of bipolar treatment. They help reduce extreme mood swings and maintain emotional balance.
- Lithium: Often considered the gold standard. Very good for preventing manic episodes and lowering suicide risk. Needs regular monitoring (blood levels, kidney & thyroid function). Many people feel more stable once their dose is well adjusted.
- Valproate (Divalproex / Valproic Acid)
Useful especially for mania, or mixed mood states. If you may become pregnant or have child-bearing potential, this option needs special discussion because of associated risks. Regular checks for liver function & blood work are important. - Carbamazepine (Tegretol): Helps in manic or mixed episodes. However, there’s risk of interactions with other medications, and rare side effects that affect skin or blood counts. It’s not a “quick fix” – monitoring is essential.
- Lamotrigine (Lamictal): Strong choice especially for preventing depressive episodes. It must be introduced gradually to lower the risk of skin rash. For many, it’s one of the better tolerated options.
Antipsychotics (Second‑Generation (SGAs))
Used when mania is present, for psychotic symptoms, or sometimes depression in bipolar disorder.
- Quetiapine, lurasidone – often preferred in bipolar depression.
- Risperidone, olanzapine, aripiprazole, ziprasidone, cariprazine — each has trade-offs in sedation, metabolic risk, activation (restlessness), or other side effects. What matters most is what fits your life: sleep, activity, side-effect sensitivity.
Antidepressants (With Caution)
Antidepressants can help with depressive phases, but they carry risk of triggering mania or rapid cycling. If considered, they should always be used alongside a mood stabilizer, with clear plans for when to stop or adjust, close monitoring, and open communication with your medical provider.
- SSRIs like fluoxetine may be prescribed, but monitoring is essential.
Anti-anxiety Medications
Benzodiazepines such as Lorazepam or Clonazepam may be prescribed short-term to address insomnia or severe agitation during a manic phase.
Medications for Bipolar Mania
When someone is in a manic episode, characterized by high energy, impulsivity, euphoria, or even agitation, medication is often a critical part of treatment. The goal is to reduce symptoms quickly and prevent the episode from escalating into a crisis.
Common medications used for bipolar mania include:
- Mood stabilizers like lithium, which remains a gold standard for managing manic phases.
- Antipsychotics, both typical (e.g., haloperidol) and atypical (e.g., olanzapine, risperidone), which help reduce manic symptoms and prevent psychosis.
- Anticonvulsants such as valproate (Depakote) and carbamazepine, which act as mood stabilizers and are often prescribed when lithium isn’t well-tolerated.
These medications work differently for everyone. It’s essential to work closely with a healthcare provider to monitor side effects and effectiveness.
Caution: Antidepressants are typically avoided or used cautiously during manic episodes, as they can trigger or worsen mania in some patients with bipolar disorder.
Medications for Bipolar Depression
Treating bipolar depression is more complex than treating unipolar depression. While the depressive symptoms, low energy, hopelessness, emotional numbness, may look similar, the treatment approach is different due to the risk of triggering mania.
Medications commonly used include:
- Mood stabilizers such as lamotrigine (Lamictal), which is particularly effective for depressive symptoms in bipolar disorder and has a lower risk of triggering mania.
- Atypical antipsychotics like quetiapine (Seroquel) and lurasidone (Latuda) are FDA-approved for bipolar depression and are often first-line treatments.
- Antidepressants may be used very cautiously, and usually only in combination with a mood stabilizer to avoid manic switches.
Each case is different, and finding the right medication, or combination of medications, can take time. Regular follow-up with a psychiatrist is essential to adjust treatment as needed and manage any side effects.
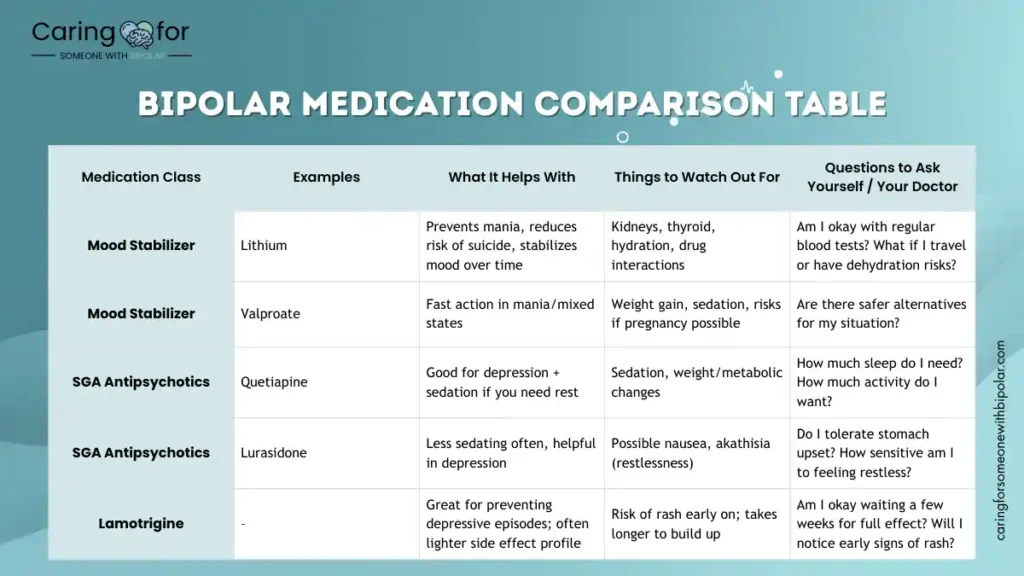
Comparison Table: What Might Suit You
| Medication Class | Examples | What It Helps With | Things to Watch Out For | Questions to Ask Yourself / Your Doctor |
|---|---|---|---|---|
| Mood Stabilizer | Lithium | Prevents mania, reduces risk of suicide, stabilizes mood over time | Kidneys, thyroid, hydration, drug interactions | Am I okay with regular blood tests? What if I travel or have dehydration risks? |
| Mood Stabilizer | Valproate | Fast action in mania/mixed states | Weight gain, sedation, risks if pregnancy possible | Are there safer alternatives for my situation? |
| SGA Antipsychotics | Quetiapine | Good for depression + sedation if you need rest | Sedation, weight/metabolic changes | How much sleep do I need? How much activity do I want? |
| SGA Antipsychotics | Lurasidone | Less sedating often, helpful in depression | Possible nausea, akathisia (restlessness) | Do I tolerate stomach upset? How sensitive am I to feeling restless? |
| Lamotrigine | – | Great for preventing depressive episodes; often lighter side effect profile | Risk of rash early on; takes longer to build up | Am I okay waiting a few weeks for full effect? Will I notice early signs of rash? |
Side Effects and Managing Medication Challenges
Medications for bipolar disorder can be life-changing, but they’re not without side effects. One of the biggest reasons people stop treatment is discomfort, not disbelief in the diagnosis.
Common side effects include:
- Weight gain
- Drowsiness or fatigue
- Tremors
- Gastrointestinal issues
- Blunted emotions or loss of creativity
It’s important to communicate openly with a healthcare provider about side effects. Never stop medication suddenly without guidance, doing so can trigger a severe relapse or withdrawal symptoms.
Practical tips for managing medication challenges:
- Keep a simple daily journal: mood, sleep, side effects, small wins. It helps you and your clinician see patterns.
- Speak up early: if something is becoming bothersome (weight changes, fatigue, mood shifts), there may be tweaks. Dose timing, switching medications, adding supportive therapy—all can help.
- Prioritize your physical health: sleep, nutrition, consistent routine. Our bodies and minds are intertwined.
- Never stop medications suddenly. Changes should be gradual and guided by your clinician to avoid relapse.
Alternative and Complementary Approaches to Bipolar Treatment
While medication and therapy remain the cornerstones of bipolar disorder treatment, many individuals explore additional strategies to manage symptoms and improve quality of life. These approaches aren’t replacements, but they can be valuable allies when integrated into a comprehensive treatment plan.
Nutrition and Supplement Support
Some research suggests that certain nutrients may help stabilize mood:
- Omega-3 fatty acids (found in fish oil) have been linked to improved brain function and reduced depression severity.
- Magnesium and folate may play a role in mood regulation.
- N-acetylcysteine (NAC) has shown promise in reducing symptoms in some bipolar studies.
Always talk to a psychiatrist before starting supplements—some may interact with prescribed medications.
Mindfulness and Meditation
Mindfulness-Based Cognitive Therapy (MBCT) and meditation practices can increase self-awareness, reduce stress, and help prevent depressive relapse.
- Apps like Calm and Headspace offer guided meditations designed for mental wellness.
- Deep breathing, body scans, and mindfulness walks are simple yet powerful tools to regulate emotion.
Exercise as a Mood Regulator
Regular physical activity is one of the most studied natural stabilizers:
- It can increase serotonin and endorphins.
- Helps reduce anxiety and improve sleep.
- Even 30 minutes of walking can support emotional balance.
Light Therapy for Bipolar Depression
Used carefully (especially under professional supervision), bright light therapy may help treat bipolar depression without triggering mania.
- It’s often combined with mood stabilizers to minimize risk.
- Timing and dosage are critical—talk to a doctor before use.
Acupuncture and Yoga
Emerging research supports the role of body-based practices like yoga and acupuncture in reducing anxiety and stress, which may reduce the intensity of mood episodes.
Note of Caution
Alternative approaches can complement, not replace, clinical care. Before adding any new modality, consult your mental health team. Some seemingly “natural” treatments can disrupt stability if not managed properly.
Learn more: What Does Untreated Bipolar Really Look Like? for a deeper look into the risks of self-managing without supervision.
Children and Bipolar Medication
Treating bipolar disorder in children presents unique challenges—and requires specialized care. Children’s brains and bodies are still developing, so what works for adults may not be appropriate for younger patients.
FDA-Approved Medications for Pediatric Use
Some medications have been approved for treating bipolar disorder in children and teens:
- Risperidone (Risperdal) and aripiprazole (Abilify) are commonly prescribed atypical antipsychotics.
- Lithium has also been used for adolescents, especially those with classic manic episodes.
These medications aim to manage symptoms while minimizing side effects—but careful monitoring is essential.
Why Diagnosis and Dosing Are Complex
Diagnosing bipolar disorder in children is difficult because symptoms can overlap with ADHD, autism, or trauma responses. Additionally:
- Children may experience rapid mood shifts or mixed states more frequently than adults.
- Finding the right dose often involves trial and error, due to body size and sensitivity to side effects.
Parent Involvement is Crucial
Parents and guardians play a central role in:
- Monitoring medication side effects
- Reporting changes in mood or behavior
- Creating structure and routines to support emotional regulation
Open communication with a child’s psychiatrist and therapist helps fine-tune treatment over time.
Behavioral Therapy and Education
Medication is often paired with:
- Family therapy
- Psychoeducation to help the child understand their emotions
- School-based supports such as IEPs or 504 plans
These wraparound strategies create a more stable foundation, both at home and in the classroom.
Resource: Supporting Children of Bipolar Parents, If you’re navigating a family dynamic affected by bipolar, this guide is for you.
When to Adjust or Change Medication
Medication for bipolar disorder isn’t a “set it and forget it” solution. Over time, symptoms may shift, side effects may develop, or life circumstances may change. Knowing when to revisit a treatment plan is key.
Signs It Might Be Time for a Change
Pay attention to these common indicators:
- Recurring manic or depressive episodes, despite taking meds regularly
- New or worsening side effects, such as weight gain, sedation, or restlessness
- Diminished effectiveness over time (called “breakthrough symptoms”)
- Emotional blunting or feeling “numb” or disconnected
If your loved one expresses frustration or concern, it’s worth discussing with their provider.
Don’t Stop or Adjust Meds Without Supervision
It can be tempting to reduce or skip doses when symptoms improve, or to stop cold turkey when side effects hit. But abrupt changes can trigger relapse, withdrawal symptoms, or dangerous mood episodes.
Always consult a psychiatrist before making changes. Some meds require gradual tapering to avoid risks.
Regular Medication Reviews
Best practice involves a medication review every 3–6 months. This helps:
- Track how well each med is working
- Reassess doses based on weight, stress, or aging
- Adjust to new symptoms or life changes
Keeping a mood tracker or medication log can help you spot trends and patterns over time.
Tip: Use a printable Medication + Mood Tracker from our Bipolar Support Toolkit to document side effects, dosage, and effectiveness.
Frequently Asked Questions About Bipolar Disorder Medication
Helpful Supports Beyond Medication
Medication is often a foundation, but not the whole story. Many people find relief and strength from:
- Psychotherapy (CBT, family therapy, interpersonal & social rhythm therapy)
- Psychoeducation – learning about your disorder helps you see early signs and engage in treatment confidently
- Routine, sleep hygiene, healthy eating, consistent schedule – small habits have big effects
- Peer support, family/friend support – talking with people who’ve been through something like what you’re going through can help you feel less alone
Recent Evidence / References
- VA/DoD Clinical Practice Guideline for Management of Bipolar Disorder, Version 2.0 (2023) — covers acute and maintenance treatment, including pregnancy/child-bearing considerations. healthquality.va.gov+2healthquality.va.gov+2
- Synopsis of the VA/DoD 2023 Guideline – helpful summary of the strength of evidence and how patient preference enters into decision-making.
Conclusion: Navigating Treatment with Compassion and Clarity
Medication is not a failure, it’s a lifeline for many people living with bipolar disorder. The right plan can offer stability, reduce suffering, and bring back a sense of normalcy. Whether you’re making decisions for yourself, your partner, or your child, remember: this is a journey, not a quick fix.
Don’t navigate it alone. Talk to doctors. Ask questions. Track progress. And stay connected to support.
Free Download
Bipolar Medication Tracker & Side Effect Log
Stay organized and empowered with our printable PDF: medication schedules, symptom logs, and doctor questions all in one place.
Download the Bipolar Medication Toolkit