There are many common misconceptions about bipolar disorder, and these myths often lead to stigma, misdiagnosis, and lack of support. This guide explores 20 myths and facts to help you understand the condition better and support loved ones with confidence.
Bipolar disorder involves distinct mood episodes – mania, hypomania, and depression – not ordinary mood swings. Misconceptions can delay care, strain relationships, and reinforce stigma. This guide clears up the most common myths with plain-language facts and practical steps caregivers can use right away.
Top Bipolar Myths (and the Facts)
Myth #1: Bipolar Disorder Is Just Mood Swings
Many assume bipolar simply means being “moody.” In reality, bipolar involves defined mood episodes, not everyday ups and downs.
Reality
Episodes of mania, hypomania, and depression last days to weeks, disrupt functioning, and are accompanied by marked changes in energy, sleep, behavior, and thinking.
Why This Myth Is Harmful
It minimizes symptoms, delays diagnosis (especially bipolar II), and fuels stigma at home and work.
Quick takeaway: Not “moodiness”, bipolar episodes are prolonged, disruptive, and medical.
What to say instead: “I know episodes are different from normal mood changes, how can I support you today?”
Myth #2: People With Bipolar Disorder Can’t Function or Be Successful
Some believe bipolar prevents a stable life. With diagnosis, treatment, and routines, many people thrive.
Reality
People with bipolar can maintain careers, relationships, and families. Public figures like Carrie Fisher and Kay Redfield Jamison show what’s possible with care.
Why This Myth Is Harmful
It reinforces stigma, invites discrimination, and discourages seeking help or disclosure.
Quick takeaway: Bipolar does not erase ambition or ability, success is possible with support.
What to say instead: “What helps you thrive when you’re well? Let’s protect those supports.”
Myth #3: Mania Is Just Feeling Happy or Energetic
Mania is often mistaken for “extra happiness.” In reality, it can be dangerous if untreated.
Reality
Mania may include racing thoughts, risky decisions, inflated self-esteem, little sleep, and sometimes psychosis. Hypomania is milder but can still be disruptive.
Why This Myth Is Harmful
Minimizing mania leads to misdiagnosis and missed safety steps.
Quick takeaway: Mania isn’t just energy, it impairs judgment and needs care.
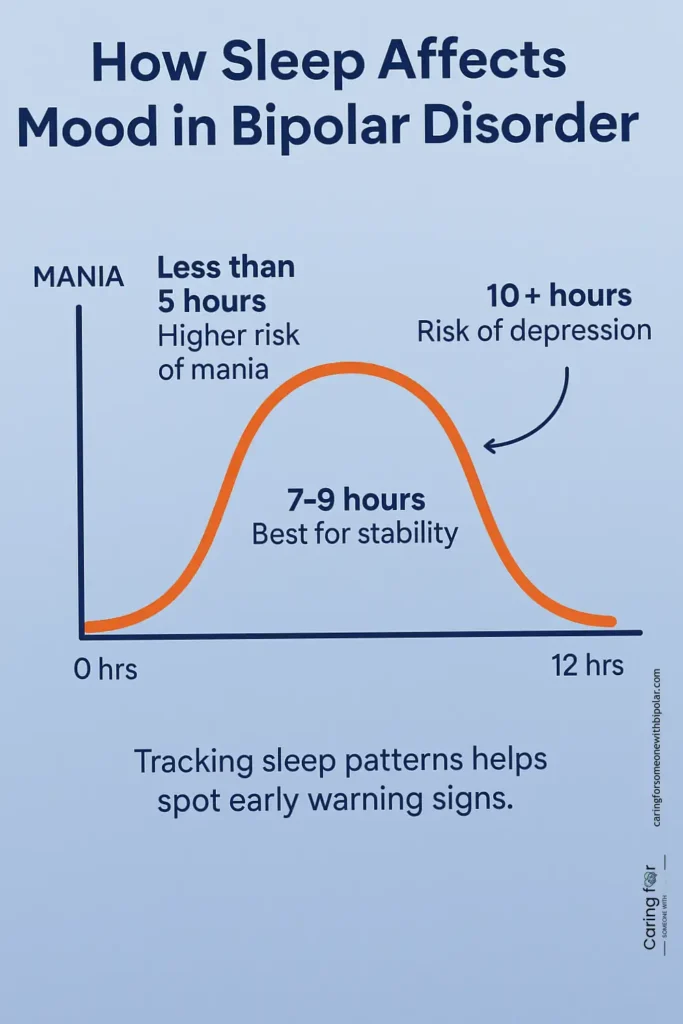
What to say instead: “Your sleep looks short, want help protecting it tonight?”
Myth #4: Bipolar Disorder Is Rare
Another misconception is that bipolar is uncommon. It’s relatively common and often underdiagnosed.
Reality
Estimates suggest ~1–2.8% of adults worldwide (some studies up to ~4%). It affects all genders and backgrounds.
Why This Myth Is Harmful
It isolates people and reduces urgency for assessment and support.
Quick takeaway: Bipolar is not rare – millions live with it.
What to say instead: “If patterns repeat, should we log mood and sleep for your doctor?”
Myth #5: People With Bipolar Disorder Are Violent or Dangerous
Media stereotypes overstate violence. Most people with bipolar are not violent.
Reality
They are more often victims than perpetrators. When aggression occurs, it’s typically linked to substance use or severe untreated episodes.
Why This Myth Is Harmful
It fuels stigma, fear, and avoidance of help-seeking.
Quick takeaway: Stigma – not danger – is the larger problem.
What to say instead: “Your safety matters, how can I support it with you?”
Safety strategies during mania
Myth #6: Bipolar Equals Borderline Personality Disorder
They’re often conflated, but they differ in patterns and care.
Reality
Bipolar mood episodes are episodic (days–weeks). BPD shifts are rapid (hours) and tied to relationships and identity.
Why This Myth Is Harmful
Confusion delays accurate diagnosis and treatment.
Quick takeaway: Different conditions → different care plans.
What to say instead: “I know these aren’t identical, have you shared your full history with a clinician?”
Myth #7: Bipolar Disorder Is Just Depression
Because depression is common, people mistake bipolar for major depression.
Reality
Bipolar requires mania or hypomania at some point. Antidepressants alone can sometimes worsen symptoms if bipolar isn’t recognized.
Why This Myth Is Harmful
Leads to misdiagnosis and suboptimal treatment.
Quick takeaway: Depression ≠ bipolar – mania/hypomania matters.
What to say instead: “This might be part of a bigger pattern – let’s keep logging it.”
Myth #8: Symptoms Are Constant Every Day
Some think bipolar means unending instability. In fact, it’s episodic.
Reality
Many experience stability between episodes, especially with treatment, sleep protection, and stress management.
Why This Myth Is Harmful
It breeds hopelessness and ignores progress.
Quick takeaway: Bipolar is episodic – stability is possible.
What to say instead: “I notice when you’re doing well too – that matters.”
Myth #9: Medication Changes Your Personality
Many fear meds will erase who they are. Proper treatment aims to stabilize mood, not personality.
Reality
With clinician oversight, medications can be adjusted to minimize side effects while maintaining balance.
Why This Myth Is Harmful
It discourages treatment, raising relapse and hospitalization risks.
Quick takeaway: The goal is balance, not changing who you are.
What to say instead: “Let’s talk with your doctor if side effects show up.”
Myth #10: You Can Snap Out of It With Willpower
Bipolar is a medical condition, not a character flaw.
Reality
Care plans often combine medication, therapy, routines, and social support.
Why This Myth Is Harmful
It adds guilt, invalidates lived experience, and delays care.
Quick takeaway: Management needs tools and support, not “willpower.”
What to say instead: “How can I help with routines or appointments?”
Myth #11: Only Adults Get Bipolar
Onset can occur in adolescence or even childhood.
Reality
Early presentations are harder to spot, so mood/sleep tracking and clinical input matter.
Why This Myth Is Harmful
It delays assessment and support for young people.
Quick takeaway: Teens can show patterns too – early help improves outcomes.
What to say instead: “Let’s track patterns and talk with a clinician.”
Myth #12: It’s Caused by Bad Parenting or Character Flaws
Bipolar isn’t a moral failing or parenting outcome.
Reality
It’s a brain-based condition influenced by genetics and biology. Family support helps management but does not cause the illness.
Why This Myth Is Harmful
Blame and shame undermine cooperation and care.
Quick takeaway: No one is to blame — focus on support and treatment.
What to say instead: “Let’s build supports that work for everyone.”
Myth #13: Therapy Doesn’t Help – Only Meds Do
Medication is often central, but therapy adds crucial skills and relapse prevention.
Reality
CBT, IPSRT, psychoeducation, and family-focused therapy improve coping, routines, and outcomes.
Why This Myth Is Harmful
It discourages effective non-medication strategies that enhance recovery.
Quick takeaway: Therapy provides tools meds can’t.
What to say instead: “Want to try building practical tools together?”
Myth #14: Antidepressants Always Make Bipolar Worse
They can trigger mania if used alone, but that’s not always the case.
Reality
Under close supervision and with mood stabilizers, antidepressants may help some people. Monitoring is key.
Why This Myth Is Harmful
It creates fear and prevents balanced treatment plans.
Quick takeaway: The risk can be managed – track response with your clinician.
What to say instead: “Let’s monitor sleep, mood, and activation closely.”
Myth #15: Bipolar Ruins Relationships
With communication, treatment, and boundaries, many couples do well long term.
Reality
Routines, shared plans, and support networks strengthen relationships.
Why This Myth Is Harmful
It promotes hopelessness and resignation instead of problem-solving.
Quick takeaway: Healthy relationships are possible with planning and support.
What to say instead: “Let’s learn what works for both of us.”
Myth #16: Substance Use Causes Bipolar
Substances can worsen episodes, but they don’t cause the disorder.
Reality
Bipolar is rooted in biology and genetics. Co-occurring substance use can trigger or intensify symptoms.
Why This Myth Is Harmful
It shifts blame and obscures medical causes and treatments.
Quick takeaway: Focus on healthier coping and treatment, not blame.
What to say instead: “Let’s find coping options that don’t worsen symptoms.”
Myth #17: Pregnancy Cures or Worsens Bipolar
Pregnancy doesn’t cure bipolar; impact varies by person. Postpartum risk can be higher.
Reality
Some improve, some worsen, some stay stable. Pre- and postpartum planning is essential; discuss medication safety with clinicians.
Why This Myth Is Harmful
It creates unrealistic expectations and neglects monitoring during vulnerable periods.
Quick takeaway: Plan care before and after pregnancy.
What to say instead: “Let’s make a shared plan with your clinician.”
Myth #18: People With Bipolar Can’t Work
Many people with bipolar build meaningful careers with support and routines.
Reality
Predictable schedules, sleep protection, and reasonable accommodations help sustain work success.
Why This Myth Is Harmful
It fuels workplace stigma and limits opportunities.
Quick takeaway: Work is possible with the right supports.
What to say instead: “What routines keep work manageable?”
Myth #19: Bipolar Is a Life Sentence Without Hope
Bipolar is chronic, but many people lead full, satisfying lives.
Reality
Treatment, support, and self-care reduce episodes and improve functioning and quality of life.
Why This Myth Is Harmful
Hopelessness undermines adherence and recovery.
Quick takeaway: Recovery is realistic with treatment and support.
What to say instead: “Let’s focus on the tools that make stability more likely.”
Myth #20: If Someone Was Fine Yesterday, They’re Faking It Today
Symptoms can shift quickly; yesterday’s stability doesn’t invalidate today’s struggle.
Reality
Rapid changes can occur within episodes or when triggers (e.g., sleep loss) stack up.
Why This Myth Is Harmful
It invalidates lived experience and reduces empathy and support.
Quick takeaway: Fluctuations are part of the illness — not “faking.”
What to say instead: “I know symptoms can change quickly — how can I support you right now?”
Quick Reference Table – 20 Common Misconceptions About Bipolar Disorder: Myths vs Facts
A. Understanding Symptoms and How Bipolar Really Works
| Myth | Fact | Why it’s harmful |
|---|---|---|
| Bipolar is just mood swings | It involves distinct episodes of mania, hypomania, or depression. | Minimizes symptoms and delays assessment. |
| Mania just means being extra happy | Mania can include impaired judgment, little sleep, risky behavior. | Overlooks safety and sleep protection. |
| Bipolar is rare | It’s not rare; bipolar II is often underdiagnosed. | Dismisses concerns and discourages assessment. |
| Bipolar is just depression | Defined by episodes of mania or hypomania, not just depression. | Causes misdiagnosis and harmful treatment choices. |
| Symptoms are constant every day | Bipolar is episodic; stability periods exist between episodes. | Discourages hope and invalidates progress. |
B. Myths About Who Gets Bipolar and What Causes It
| Myth | Fact | Why it’s harmful |
|---|---|---|
| People with bipolar are violent | Most are not; they’re more often victims of violence. | Reinforces stigma and social exclusion. |
| Only adults get bipolar | It can appear in adolescence or childhood. | Delays early care and intervention for young people. |
| It’s caused by bad parenting or flaws | It’s biologically and genetically rooted, not caused by parenting. | Blames families and increases shame. |
| Substance use causes bipolar | It can worsen symptoms but does not cause bipolar disorder. | Shifts blame and ignores medical origins. |
| Pregnancy cures or worsens bipolar | Pregnancy does not cure it; postpartum is higher risk. | Leads to unsafe expectations and neglect of monitoring. |
C. Treatment, Medication, and Recovery Myths
| Myth | Fact | Why it’s harmful |
|---|---|---|
| Medication changes your personality | Proper treatment balances symptoms without erasing identity. | Creates fear of treatment and relapse risk. |
| You can snap out of it with willpower | It is a medical condition requiring treatment and support. | Invalidates lived experience and adds guilt. |
| Therapy doesn’t help | Therapies (CBT, IPSRT, psychoeducation) improve coping and recovery. | Discourages helpful non-medication strategies. |
| Antidepressants always make bipolar worse | They may help when used safely with mood stabilizers. | Creates fear and prevents balanced treatment. |
| Bipolar is a life sentence without hope | Recovery and stability are possible with care and support. | Promotes hopelessness and treatment avoidance. |
D. Work, Relationships, and Daily Life Myths
| Myth | Fact | Why it’s harmful |
|---|---|---|
| People with bipolar can’t live normal lives | Many maintain careers, relationships, and parenting with support. | Fuels stigma and discourages treatment. |
| Bipolar equals borderline personality disorder | They are distinct conditions with different patterns and care. | Leads to misdiagnosis and wrong treatment. |
| Bipolar ruins relationships | With support and boundaries, healthy long-term relationships are possible. | Promotes hopelessness for couples. |
| People with bipolar can’t work | Many succeed at work with treatment and support routines. | Creates workplace stigma and discouragement. |
| If fine yesterday, faking today | Episodes can shift quickly; fluctuations are part of the illness. | Invalidates the person’s lived reality. |
Comparisons
Bipolar I vs Bipolar II vs Cyclothymia
| Feature | Bipolar I | Bipolar II | Cyclothymia |
|---|---|---|---|
| Defining episode | At least one manic episode (with or without depression) | Hypomanic episodes + at least one major depressive episode | Chronic hypomanic and depressive symptoms not meeting full criteria |
| Impairment | Often marked; may require hospitalization | Noticeable but usually less impairing than mania | Functional impact varies; long fluctuating course |
| Psychosis risk | Possible during mania or depression | Less common than Bipolar I | Uncommon |
| Depression | Common but not required for diagnosis | Required (major depressive episode) | Subthreshold depressive symptoms are frequent |
| Typical misreads | “Just high energy,” ADHD, substance-related | “Just depression,” anxiety disorders | “Moodiness,” personality or situational |
| Caregiver watchouts | Sleep loss, risky behavior, grandiosity, psychosis signs | Sleep/schedule drift, activation after antidepressants | Pattern tracking over months, stress-sleep links |
Tip: If episodes repeat over days-weeks, ask a clinician about bipolar assessment and bring a mood/sleep log.
Mania vs Hypomania vs Mixed Features
| Feature | Mania | Hypomania | Mixed Features |
|---|---|---|---|
| Mood/energy | Elevated/irritable with marked overactivity | Elevated/irritable; noticeable increase in activity | Concurrent manic and depressive symptoms |
| Sleep | Dramatically decreased need | Decreased need | Disturbed, restless, poor quality |
| Functioning | Often impaired; may need hospitalization | Still functioning but off baseline | Highly distressed; functioning can drop quickly |
| Risks | Financial/sexual/legal risks; psychosis possible | Impulsive decisions; conflict | Higher suicide risk; agitation + despair |
| Caregiver actions | Reduce stimulation; protect sleep; safety plan | Support routines; watch sleep; de-escalate | Prioritize safety; seek urgent clinical input |
Learn practical steps for each state: During mania · During depression.
Bipolar vs BPD vs ADHD vs MDD
| Dimension | Bipolar Disorder | Borderline Personality Disorder (BPD) | ADHD | Major Depressive Disorder (MDD) |
|---|---|---|---|---|
| Pattern of change | Episodic (days–weeks) mood episodes | Rapid shifts (minutes–hours), relationship-triggered | Persistent inattention/hyperactivity (since childhood) | Depressive episodes (weeks), no hypomania/mania |
| Core triggers | Biology, sleep loss, stress, substances | Interpersonal stress, abandonment sensitivity | Neurodevelopmental; situational stress worsens | Psychosocial/biological stressors |
| Sleep | Decreased need in mania/hypomania; variable in depression | Variable (often poor during crises) | Variable; often delayed sleep, irregular schedules | Often increased or decreased; early waking common |
| Self-image & relationships | Not core to diagnosis; strain during episodes | Identity disturbance; intense, unstable relationships | Not central; executive/organization impairments | Low self-worth during episodes |
| Course over time | Recurrent episodes with inter-episode recovery | Chronic interpersonal/affective instability | Chronic pattern; improves with management | Episodic; may recur |
| Caregiver focus | Track episodes; protect sleep; safety planning | Validation skills; boundaries; crisis plan | Executive supports; routines; reminders | Safety checks; activation; professional care |
Not sure which pattern fits? Keep a simple daily log and share with a clinician.
Caregiver Toolkit
Early-Warning Signs & Triggers Checklist
Use this quick checklist to spot patterns early and act before a full episode develops. Share it with your clinician if patterns repeat.
- Sleep loss or staying up later than usual
- Sudden increase in goal-directed activity or spending
- Irritability, agitation, or unusual risk-taking
- Racing thoughts, pressured speech, reduced appetite
- Withdrawing, hopelessness, fatigue, slowed movements
- Substance use or medication changes
- Major stressors (conflict, travel, shift work, exams)
Language Swaps That Reduce Stigma
Small wording changes build trust and reduce defensiveness. Try these alternatives.
| Avoid saying | Try instead | Why it helps |
|---|---|---|
| “Calm down.” | “Let’s try a grounding exercise together.” | Invites collaboration and regulation. |
| “You were fine yesterday.” | “I know symptoms can change quickly. How can I support you now?” | Validates fluctuations without blame. |
| “Why are you like this?” | “Today looks heavy. What would help right now?” | Shifts from judgment to support. |
| “Just use willpower.” | “Managing bipolar takes tools and support. I’m here to help.” | Affirms it’s a medical condition. |
Gentle Check-In Scripts (Text / Call / In Person)
Text message:
- “Noticing you’re sleeping less. Want help protecting sleep tonight?”
- “If today feels intense, we can make a simple plan together.”
- “I’m around at 7 if you want a quick check-in.”
In person:
- “Would a quiet walk or a grounding exercise help right now?”
- “Do you want me to handle dinner so you can rest?”
Follow-up (next day):
- “How did last night go? Anything we should adjust today?”
Bipolar Emergency Plan (Step-by-Step)
Create a written plan you can use during high-stress moments. Review it when well.
- Contacts: clinician, emergency services, trusted family/friends
- Medications: current list, dosages, allergies
- Safety steps: reduce stimulation, remove access to high-risk items, transport plan
- Care logistics: work/school note, child/pet care backup, finances
- Consent & boundaries: what information can be shared, with whom
- Hospital preferences: nearby facilities, insurance details
During Mania: Safety-First Actions
- Protect sleep: reduce stimulation, agree on a wind-down routine
- De-escalate: keep voice calm, avoid arguments or ultimatums
- Safety: delay major decisions (spending, travel), limit driving if impaired
- Escalate care if needed: contact clinician or crisis services
During Depression: Practical Supports
- Basic care: meals, hydration, gentle movement, sunlight
- Structure: small tasks, low-pressure plans, compassionate pacing
- Safety: check for hopelessness; know when to escalate care
Daily Mood & Sleep Tracking
Simple logs help spot patterns and guide treatment decisions. Share summaries with your clinician.
Download our printable tracker
Boundaries & Consent for Caregivers
- Agree on what support is welcome (and what is not)
- Set limits on finances, safety, and crisis steps
- Clarify privacy and information-sharing preferences
- Revisit boundaries after episodes to refine the plan
Read boundary & consent guidelines
Download the Caregiver Toolkit (PDF)
Get printable checklists, scripts, and the emergency plan in one file.
📌 What are the common misconceptions about bipolar disorder?
Common misconceptions about bipolar disorder include the belief that it’s just mood swings, that people with bipolar are unstable or dangerous, or that the condition is rare. In reality, bipolar disorder is a serious but treatable condition affecting millions, and many individuals lead successful, stable lives.
What Bipolar Disorder Is Often Confused With
Because bipolar disorder includes a wide range of symptoms that can appear in different ways, it is often confused with other mental health conditions. This can lead to misdiagnosis and delayed treatment, especially during the early stages of the illness.
Commonly Misdiagnosed Conditions
- Major Depressive Disorder (MDD)
Many people with bipolar disorder first seek help during a depressive episode. Without a clear history of mania or hypomania, they are often diagnosed with depression alone. This is especially common in cases of Bipolar II. - Attention-Deficit/Hyperactivity Disorder (ADHD)
Both conditions can involve impulsivity, distractibility, and mood variability. In children and teens, bipolar disorder is sometimes mistaken for ADHD, particularly when symptoms of hyperactivity and poor concentration are present. - Borderline Personality Disorder (BPD)
Bipolar and BPD both involve emotional instability, intense relationships, and mood swings. However, bipolar mood episodes are more prolonged and cyclical, while BPD symptoms are more reactive to environment and interpersonal stressors. - Substance-Induced Mood Disorders
Symptoms of mania or depression caused by drug use can mimic bipolar disorder, making it difficult to distinguish the root condition until substances are no longer a factor.
Why Accurate Diagnosis Matters
Misdiagnosis can lead to:
- Inappropriate medications that worsen symptoms
- Lack of proper mood stabilization strategies
- Confusion and frustration for both patients and their families
Clear evaluation by a qualified mental health professional is essential. This often includes a full psychiatric assessment, detailed symptom history, and collaboration with close family members or partners.
Breaking the Stigma: What You Should Know
Common Misconceptions About Bipolar disorder don’t just create confusion, they fuel stigma that harms individuals, families, and communities. Breaking that stigma begins with education, empathy, and a willingness to listen.
Education Reduces Fear
Many people fear what they don’t understand. Learning about bipolar disorder from reliable sources helps dismantle harmful assumptions. Schools, workplaces, and families all benefit when mental health is treated as a legitimate medical topic rather than a personal failing.
Language Matters
Casual phrases like “I’m so bipolar” or calling someone “crazy” reinforce stigma. Replacing judgment with respect can reshape how we talk about mental health in daily life.
Examples of stigma-free language:
- “They’re managing bipolar disorder” instead of “They’re unstable”
- “She has a diagnosis of bipolar” instead of “She’s bipolar”
Support Creates Change
The most powerful way to break stigma is through compassionate connection. This includes:
- Listening without judgment
- Encouraging professional help
- Learning how to support someone living with bipolar disorder
By challenging stereotypes and sharing facts, we can reduce shame and help people feel seen, supported, and empowered.
Frequently Asked Questions About Bipolar Disorder
Concise answers to common questions. Click a question to expand.
What are the most common misconceptions about bipolar disorder?
Can someone with bipolar disorder live a normal life?
Is bipolar disorder the same as borderline personality disorder?
What’s the difference between bipolar I and bipolar II?
Does bipolar disorder get worse with age?
Can bipolar disorder be cured?
Are people with bipolar dangerous?
How is bipolar disorder diagnosed?
What triggers bipolar episodes?
Does therapy help or is medication enough?
How can family support someone with bipolar?
What are some stigmas associated with bipolar disorder?
What is the most common misdiagnosis of bipolar disorder?
How does a person with bipolar think?
What could be confused with bipolar?
Conclusion: Understanding Bipolar Means Letting Go of Myths
Bipolar disorder is a complex and deeply personal condition that affects millions of people worldwide. Unfortunately, many individuals carry not only the weight of their symptoms but also the burden of widespread misunderstanding.
By learning the facts and addressing the common misconceptions about bipolar disorder, we can begin to replace fear with empathy, and stigma with support. Whether you’re living with bipolar disorder or supporting someone who is, debunking these bipolar myths empowers better conversations, stronger relationships, and healthier outcomes.
What You Can Do Next
- Share this article with someone who may need clarity
- Continue learning: explore our guide on the [Types of Bipolar Disorder]
- For support strategies, visit: [How to Support Someone With Bipolar Disorder]
When we replace myths with understanding, we create space for real healing.
Call To Action
Understanding bipolar disorder starts with breaking the myths, but true support goes further.
Download our free Caregiver Toolkit, use the mood tracking template, and explore our guides for practical ways to help your loved one every day.
You don’t have to do this alone.
Take the Next Step: Free Caregiver Toolkit
Understanding bipolar myths is only the first step. Get our free Caregiver Toolkit (PDF) packed with checklists, scripts, and trackers to support your loved one effectively.
📥 Download Toolkit (PDF) 📝 Mood Tracking Template
Examples for mood:
* Manic/hypomanic: feeling “up”, jumpy, irritable, racing thoughts
* Depressive: sad, fatigued, low energy, difficulty concentrating
Clinically reviewed by [Nom], [Titre], [Date]